I.
When Reem, a Sudanese woman in the besieged North Darfur capital of El Fasher, arrived at the Saudi Specialized Hospital for Obstetrics & Gynecology, the last maternity hospital left here during Sudan’s year-long civil war, on 19 May 2024, she required an emergency cesarean section.
Like clockwork, the maternity team registered her, discovered her pregnancy was blocked, likely due to previous scarring, and moved her to the operating theater. That’s when the physicians of Unit #4, known as the “Butterfly Unit,” took over.
Dr. Samar, along with a team of nurses, an anesthesiologist, and others, performed the surgery. Samar’s team made the incision, delivered the baby and placenta, closed the wound, and the mother now had Darfur’s newest child.
But just after Dr. Samar’s team moved Reem and her newborn from the operating theater to the recovery room, there was an enormous explosion, blasting the windows out across the surgical theater and nearby rooms.
“That was the most terrible position I ever faced in my life,” Samar remembers, bracing herself. Her fellow “Butterfly Unit” doctor, Dr. Aisha Hassan, was just in the next doorway.
“The force of the explosion broke every window around the area where people were conducting surgery,” Aisha recalls. “It was like being hit by lightning. Every person at the hospital was in shock. I just stood there in place. I didn’t even run or anything. The explosion injured eight people. We had to perform first aid and then transfer them to the South Hospital.”
Dr. Modther Ibrahim Suleman, the Saudi maternity hospital’s young, bespectacled medical director, who had known Samar and Aisha since school, quickly assessed what had happened. Everyone knew that the Sudanese government, which had spent two decades building its Rapid Support Forces (RSF) largely with Arab Baggara tribal militias from around Darfur, now faced those same forces who had turned against them countrywide.
By May 2024, the RSF had taken most of Darfur, surrounding the city of El Fasher. Over the next six months of fighting, Sudan Armed Forces (SAF) and the Joint Forces (JF) supporting them in a temporary alliance dug in and held their positions but could do little to stop the RSF from firing on civilian positions.
Until this direct hit on the maternity hospital, the medical teams of El Fasher had remained optimistic, hoping and praying that no fighters would ever target a health center. Modther informed allies of what had just happened, sending images of the broken water tank, generator, and shattered glass.
“I’m very sad to tell you that a bomb hit the maternity hospital today,” he wrote to this writer, “a rocket shell. There were nine injuries, three of them serious—passersby and merchants outside the hospital. Please, if you can, let the world know.”

In the coming months, Sudan’s year-long civil war would lead to six months of violent siege for El Fasher. Fighters would bombard the maternity hospital at least 16 separate times, alongside attacks on nearly every hospital and health center across town. The war was escalating, and in this war, hospitals were no longer safe.
Very quickly, Modther’s team of obstetric and gynecology specialists would be forced to transform this modest maternity hospital into the region’s last emergency war hospital.
In the fighting to come, El Fasher’s one million residents would be cut off from their water supply, food convoys, and even aid, creating famine conditions as the government and RSF fought for control.
As international aid agencies largely withdrew and ran out of funding, local Sudanese medical teams would be forced to save lives under fire with shrinking supplies. Some would be killed, many wounded, many evacuated, and still others would have to keep this war hospital running under some of the toughest conditions in history.

II.
When we started this story, we wanted to understand how Sudanese medical teams save lives on the frontlines and what the international community could do to provide them with more support, especially in light of the dramatic global rise in attacks on health workers as reported by Insecurity Insight alongside the Safeguarding Health in Conflict Coalition.
But we had not anticipated how quickly most of the international community would withdraw, leaving local Sudanese doctors very little support as they provide healthcare under harrowing conditions. Opportunities to arrange air drops of supplies or transfers of funding for local purchases have been largely held up by donor fatigue and bureaucracy at a violent time.
While interviewing Modther, his team of doctors of Saudi maternity hospital’s Unit #4, as well as other surgeons, trauma medics, aid workers, and survivors remotely from Berlin, Germany, this writer worked with photographer Mohamed Zakaria, referred to here as Mo, reporting on the ground. Early in the siege, Mo produced visual documentation of the war in his native El Fasher for the BBC, which agreed for him to provide photos for this story and assist with additional reporting.
Mo, a tall, confident visual artist with a serious demeanor alongside a warm sense of humor, had grown up in El Fasher. He met Modther in the same circles where Samar and Aisha spent time, and then met another media colleague, Mohamed Faisal, known as Keeta.
Together Modther, Mo, and Keeta would propose making films together about life in Sudan. They wanted to show how the western region of Darfur was recovering from the troubles of past decades, how technology, the arts, and diversity were coming to their rapidly growing city.
That led to the creation of their production company, Dar Productions, which would host media teams to cover health services in the region. But they never imagined this collaboration would lead them to be among the last in El Fasher to tell the world what was happening when war broke out.
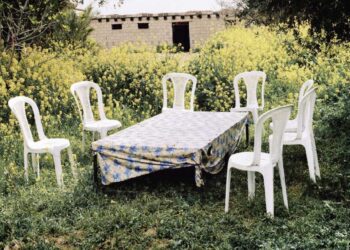
Over the past years, media companies ranging from CNN to Al Jazeera had come to El Fasher to capture video and photos—not always of the city’s thriving market and green oasis barbeques, but more often of the massive displaced family settlements on the scorched edges of town, or the clinics and field hospitals in Zamzam, telling the world about desertification and its impact on displaced survivors of the earlier war and hunger. Mo would grab his camera and gimbal, Keeta would arrange the clients, and Modther would help the media connect with hospital or aid agency staff for interviews.
But when the war broke out and the siege drew closer, Modther shifted all his focus to the medical response, serving as medical director at the Saudi hospital with general manager Sami, their staff, and an increasing number of volunteers who wanted to help—many of whom had lost their homes and sought shelter nearby, eager to contribute. Meanwhile, Keeta went abroad with his family, and Mo decided to apply his skills as a war photographer and stayed with his camera ready even as the war surrounded them.
On 11 May, just as Modther, Mo, and I agreed by phone to produce a story series on El Fasher’s local medical teams, fighters bombed the Babiker Nahar Pediatric Hospital, killing one staff member and two children, and knocking the hospital out of service.
The following week, fighters also hit the Saudi maternity hospital and fully encircled the city. In one of our first talks about the war they were witnessing on the ground, Mo told me there were dead bodies in the street. Shortly after, he sent a video of the smoke plume from a mortar or rocket that had detonated not far from where he had taken cover.

III.
Long before Sudan’s civil war erupted in April 2023, Darfur had endured waves of ethnic violence. El Fasher, the capital of North Darfur, however, had long been seen as a bastion of hope and one of the safer, multicultural communities. Families escaping ethnic violence across the region, if they didn’t escape across the border, would come here.
The Sudan Ministry of Health (MoH), led by Director General Dr. Ibrahim Abdullah Khatir and South Hospital’s medical director and top surgeon, Dr. Izzeldin Asow, faced difficult choices in this fragile environment.
MoH teams aimed to provide healthcare impartially, treating civilians and military personnel alike, regardless of ethnicity or religion. However, as the international community condemned the Sudanese government, the Rapid Support Forces (RSF), and the overlapping janjawid militias (devils on horseback) for their roles in ethnic violence, including during the 2003-2008 Darfur War and 2013 Darfur clashes, ensuring equal healthcare for all became increasingly difficult. Some international donors even boycotted health centers linked to the government.
Medical teams, including those led by Dr. Izzeldin Asow, the medical director at South Hospital, the main medical center, and Dr. Modther, medical director at Saudi Maternity, faced a dilemma, whether to serve the city’s urban elite or join humanitarian clinics supporting thousands of displaced families in surrounding areas like Zamzam and Abu Shouk.
International aid agencies and local health workers had set up field hospitals and women’s clinics on the outskirts, while South Hospital, with help from organizations like Doctors Without Borders (MSF) and Relief International (RI), became a hub for specialized care. Soon, the “Butterfly” women’s health teams began rotating through these hospitals as staff was limited and the medical community agreed together to cross-train staff to be sure they could cover each other’s roles when needed as the war approached.
Within this context, the Saudi maternity hospital team stood out. Led by Modther and his general manager Sami, this highly organized team—composed largely of women—treated pregnancy complications such as eclampsia, hypertension, and hemorrhaging, as well as gynecological issues ranging from fistula infections to wounds from rape and sexually transmitted diseases.
Before the war, Saudi Maternity was seen by many as a feminist team in a conservative society, which put many medical staff in the awkward position of representing Islamic, traditional, and family values while at the same time offering women and girls advice, when asked, about how to cope with rape, domestic violence, early pregnancy, or being disowned because of a feminine health struggle. This was where girls who had been raped or had humiliating infections went quietly, sometimes unable to return to their families.
Despite the stigma, the maternity staff, including Unit #4 pushed through chauvinism to focus on the beauty of nafeer—the tradition of working together for a common cause—and helping women of any background survive childbirth and witness their newborns’ first breaths.
When one entered the wide orange and pink stone halls of Saudi hospital, one found Modther there, his contagious smile reminding everyone of unity and commitment. He would stay at his station or desk as long as necessary to keep the place running smoothly, even when the Starlink satellite internet faded, the generator or solar power waned, or he hadn’t eaten since morning.
Working alongside Modther, there was Dr. Samar, the quiet one, who had known Modther since secondary school and was there the day the first bomb hit their hospital. There was Dr. Aisha Hassan, an only child whose mother had pressured her to become a doctor, but who had grown to love it. She met Samar and Modther at university.
There was Dr. Eilaf Mohamed, the one with the huge smile who liked to crack jokes to keep everyone’s spirits up. And there was Dr. Afrah Hussein, among many others. Afrah was the sweet one, full of emotion.
Who wouldn’t react full of emotion after seeing mothers cross the desert to reach the hospital with complications, witnessing their children survive, and then fearing rockets could crash through the windows at any moment?
“During the war,” Dr. Eilaf recalls, “the maternity hospital team was the most unified of all. They did their work with love. Everyone there was there because they wanted to give back to society, to help women—not because it was just their job or because they had to.”
“Kind and helpful colleagues,” Dr. Afrah remembers. “The beautiful ‘Butterfly Unit’, Unit #4. We called our unit the ‘Butterfly Unit’ because we were all women—house officers, medical officers, and registrars. We worked with love, and the hospital became our safe haven, our warm home where we worked, learned, and had fun. We formed a family.”
Both then and now, as their journeys have taken them in very different directions, the Butterflies remain united as friends—among the rare few who literally had to deliver babies during artillery barrages.
“We had the best team at the maternity hospital,” Aisha told me during a call. “The work environment was dynamic and allowed us to be close. Every team knew what to do. For example, we had a patient with a ruptured placenta. It had separated from the uterus—an ectopic pregnancy. She was hemorrhaging and had lost so much blood, so we arranged for surgery.
“Then she had postpartum bleeding and lost more blood, going into shock. We gave her life-saving drugs. Some prepared blood. Thanks to our teamwork, she survived and was doing well. When you have a good working environment, you can accomplish anything.”

IV.
A few weeks before the surgical theater blast, Aisha, Samar, and Eilaf met during a break in the courtyard area. Eilaf made a call to check on friends, then checked on a new mother with her infant, and returned to take a seat outside.
“That’s when I heard the sound of the bullet coming through the ceiling,” Eilaf remembers. “I tried to move, but it happened in the blink of an eye, in the spark of a second… I had believed the war would never come near a hospital, that soldiers would never treat a hospital as a target.”
“Suddenly, a stray bullet flew in and hit her ankle,” Aisha told me. “It was a very hard moment for us. It could have hit her anywhere—her head or her chest. She was very brave to endure that pain and remain patient about what happened. We provided first aid and then transferred her to the South Hospital, which was the main hospital at the time. We were in shock.”
By that time in mid-April, the RSF had already taken most of Darfur and surrounded the city of El Fasher, as well as the nearby mountain enclave of Jebel Marra.
On 10 May, the RSF officially closed the siege line, blocking the roads and water sources, then attempting to penetrate the SAF lines through the displacement settlement on the north side of the Abu Shouk neighborhood.
The next day, fighters—though it is still disputed who fired this early round—hit the Babiker Nahar Pediatric Hospital, killing one staff member and two children, and forcing the hospital to close. At the time, Dr. Abubakr Abdulla, another colleague from the medical circle, contacted Mo and then told me what had happened over the phone.
“After the fighting started, the pediatric hospital was too deep in the war zone,” Dr. Abubakr told us. “The first bomb hit the yard in front of the hospital. Everything there collapsed inside. Even the doors were bent inward. There were many injuries and one immediate death (the others died later).
“I was in the operating room when the bomb hit the hospital floor,” Abubakr continued, “and we had a difficult time. Everyone panicked, so we built a wall from the inside just to protect ourselves. The war zone was too close to the hospital. Then the hospital manager decided to evacuate.”
As the siege intensified, Modther would call me and other allies and media to update us on the worsening situation. On 13 May, Modther was again in shock.
“The situation is very bad. Three days of fighting, many victims and injuries. Many people were shot in my hospital—I think by a sniper or misfire. And many bombs have fallen nearby. We are still working. Unfortunately, three or four bombs fell in front of the house where my family had relocated. Fortunately, no one was injured. Also, yesterday while I was driving near South Hospital, a sniper tried to shoot my car!”
“Imagine working under the sound of bullets,” Afrah later reflected on this time, “with the hopes of many people pinned on you—sometimes succeeding, and at other times failing to save them. Those were sad days, filled with the smell of death and sorrow…”
Increasingly, as Sudan’s economy was already strained by extreme disparity, desertification led to worsening droughts, punctuated by shock floods that destroyed houses and brought malaria. Then, the war filled with undisciplined soldiers, and the Butterflies’ patient outcomes didn’t always go as well.
Eilaf recalls numerous women with fistula whose families turned against them due to the stigma. Aisha remembers rape survivors who had to sneak in to ask questions they could never pose to their families.
In a harrowing example of how war worsens health outcomes, one young woman, whom Eilaf remembers well, arrived just as the war drew near. She had gotten pregnant by accident and, fearing family judgment, attempted to end the pregnancy herself.
Tragically, she broke the stick she had used. The maternity teams rotated, some conducting investigations, finding the particles, attempting to remove them, and offering her dialysis. But by then, the war was so close that supplies had run out, power was failing, and there were too many wounded to tend to all the resident patients.
Amid the chaos, the young woman died. The Butterflies, keeping each other positive, carry these painful memories as they strive to move forward.
On the other side of town, not far away, Eilaf was recovering from the bullet wound in her foot.
“Actually, nowhere is safe now in El Fasher,” Eilaf told me over the phone. “Even the hospital is not safe. I don’t know if Modther told you. It feels like inevitable death here because there is no way to escape it. I just feel like someone is going to die, that I’m going to die in the next second, the next…”
Her voice was then interrupted by four very loud close booms I could hear over the line.
“I don’t know if you can hear this or not, but it’s terrifying.”

V.
Dr. Izzeldin Asow, the dedicated surgeon from Khartoum who quickly rose to become the beloved medical director at South Hospital—the main hospital for emergency trauma cases, orthopedic fracture care, and primary care—was under immense pressure.
“During one day,” Dr. Izzeldin told me about the beginning of the siege, “we received about 150 injured patients. In the same surgical unit, we performed general, orthopedic, and pediatric surgery in one theater, which contained two rooms. We did it harmoniously. We treated all patients without discrimination.”
Izzeldin coordinated with Ministry of Health Director General Dr. Ibrahim on one hand, his best surgeons, Dr. Fowzi and Dr. Rahman, on the other, and also with the heads of the other surviving health centers, including Modther at maternity, Dr. Khalid at Al Shuhada, Dr. Asiya at Abu Shouk, and others.
Doctors Without Borders (MSF), for their part, had helped to build and advance South Hospital’s core emergency services and skills training while also expanding their field hospital in Zamzam and maintaining clinics on the RSF-controlled side of the line.
Christos Christou, the MSF international president, regularly appeared in the news and on social media, visibly exhausted, calling for an end to attacks on hospitals and health workers not only across Sudan but also in Palestine and many other countries.
Relief International (RI) also had to evacuate expatriates and shift resources, but continued to help with ambulance services and supplies and remains one of the few international organizations working on both sides of the siege line. RI Country Director Kashif Shafique was eager to get into Sudan, but security was so bad that he had to aim first for Port Sudan, while his local team managed with limited resources.
Saif Al Yazal, the Country Director for the Darfur Peace & Development Organization, whom I had met through DPDO founder Suliman Giddo, had introduced me to Modther early on, as his team attempted to provide health assistance to a field clinic outside Abu Shouk and clean water to the maternity hospital, now had to brace as fighters bombed their flagship, the Subsaharan University College, eventually destroying it completely.
While writing this story, I reached out to a women’s health specialist at the International Rescue Committee (IRC), which had shifted its efforts toward other regions. The specialist was bringing the case of El Fasher’s women’s health to the Inter-Agency Standing Committee on sexual and reproductive health.
After a week of deliberating Sudan alongside Palestine, Myanmar, and so many other emergencies, they told her the best they could do was add a paragraph about it in their newsletter. Sudan women’s health, especially in Darfur, which was once the headline of human rights rallies and causes all over the world during the long failed “Save Darfur” movement was now out-prioritized by so many other women’s health emergencies around the world, the embattled Saudi maternity hospital, bombarded and starved, was now considered too far down the list.

When I contacted Christine Wille, director of Insecurity Insight (II), one of the leading organizations tracking threats to health works worldwide, advocating alongside the Safeguarding Health in Conflict Coalition (SHCC). She assured me that her coalition and organization were deeply concerned, yet none in their alliance had the power to act during the violence, only long before, or after the smoke had settled.
“The international community should approach these attacks on healthcare,” Ms. Wille said, “through prevention, response, and lessons learned. There is a need to support attacked health facilities in the aftermath by providing as much emergency response as possible. However, the possibilities are somewhat limited if the appropriate structures were not in place. It is particularly important that the international community does not simply move on, but takes stock of what happened, why, and how the consequences could have been prevented.”
However strong the SHCC, II, and related WHO offices advocated on health worker safety in the longer run, there remained no clear UN or INGO or safety office which could just get on the phone to advise Dr. Izzeldin, Modther, and others on how to better prepare bomb shelters, reinforce walls, or train staff on safety in these situations while the bombs were hitting.
While all this was happening, the Butterflies and other medical units rotated between health centers in El Fasher on 24-hour shifts. Among them was a young medical volunteer named Sajida Abdullah Al Mouli. On 23 May, Sajida headed to support the Emergency Response Rooms at a clinic on the edge of Abu Shouk when fighters attacked, and she was killed by a stray bullet.
After this, the Butterflies and many other medical staff faced the toughest decisions of their lives: whether to stay and serve their community or escape and take their families to safety.
Eilaf, who had already been wounded, grabbed her mother and sister, who were initially reluctant, and slipped out before the RSF fully closed the roads. Eilaf made her way to South Sudan and then onward to Uganda, while Aisha followed suit.
Meanwhile, Afrah escaped west past Tawila to the Chad border, and Samar left for another region. Among the Butterflies who stayed at the Saudi hospital working with Modther was another close friend named Eman. She made a commitment to herself to stay as long as she could. Now the Butterflies were spreading out between at least five countries, those outside calling for support when possible to those who stayed behind.
In the coming days, even Mo, who was filing stories for the BBC and saving images of the health teams for our story series, helped a wounded neighbor, only for their car to be hit by an explosive, wounding him, as well.
“These days are so difficult—the shelling is everywhere,” he wrote to me as he weighed his options: whether to stay when he could barely cross the neighborhood safely or to escape with friends. “See you tomorrow, inshallah.”

VI.
On 8 June, Dr. Izzeldin and Dr. Ibrahim Abdallah were overseeing the evacuation of South Hospital. Fighting had already come too close, international agencies and governments were unable to help, so they chose to begin moving patients to different parts of the city.
They evacuated many stable patients to the Al Shuhada health center, while the war hospital responsibilities would have to be absorbed by Modther’s team at the Saudi maternity hospital. However unprepared they were, there was no other way. MSF and RI were closeby but spread too thin to do much more than advise and offer dwindling supplies.
“Every day, the war came nearer to us,” Dr. Izzeldin recalls. “We knew this because bullets penetrated the walls of the operating theater, the outpatient clinic, and so on. One day, while we were operating on a patient, a bullet penetrated the walls, and many fragments fell on the patient while we were working on him.”
“On 8 June, Dr. Ibrahim (Abdallah) from the Ministry of Health and I came to the Saudi Hospital to prepare the backup theater room. When we returned to South Hospital, we found intense, massive shooting—bullets everywhere.
“We didn’t know the RSF would come so close to the hospital like that,” Dr. Izzeldin told me. “Suddenly, as we stepped out of the office, we heard women shouting and crying. Dr. Ibrahim and I moved forward to see why they were crying. Suddenly, we found RSF military in front of us, and they asked Ibrahim, ‘Are you civilians?’”
Izzeldin explains how the destruction alerted not only the few doctors and staff helping with evacuations but also bedridden patients, post-op patients, and those with disabilities. Some were climbing out of beds, while others pulled wheeled beds to bring their sick or wounded neighbors to safety.
Dr. Fowzi, one of the more well-known surgeons, rumored to have been beaten, escaped, but according to Izzeldin, was badly injured while jumping over the outer wall. It took him weeks to recover.
RSF fighters beat and threatened Izzeldin and Ibrahim Abdallah, according to Izzeldin, and left them for dead. Somehow, they managed to get back up, lurch back to the Saudi maternity hospital, and, after some time to recover from the trauma, resumed providing services.
Amid all this drama, Relief International team member Musa Adam Suliman had, just a few days earlier, driven to the Zamzam displacement settlement and brought back a pregnant woman with complications. But as he was driving toward the Saudi maternity hospital, a fighter shot him through the vehicle window, hitting him in the chest.

Witnesses eventually brought him to South Hospital to wait for surgery that could have saved him. However, the attack on the hospital that night complicated his situation, leading to his passing. Kashif, a deeply caring director, not only released the usual mourning news statement but also appeared in video interviews, visibly exhausted and devastated.
El Fasher’s violent situation had become so complicated that the international media made an incredibly bizarre and unfortunate decision.
While Mohamed Zakaria, now escaping overland through South Sudan, and I had been keeping up with multiple hospitals—South Hospital, Saudi Hospital, the university teaching hospital, Al Shuhada, Al Iqrah, Zamzam field hospital, and the military hospital–and with Dr. Izzeldin’s evacuation of patients to consolidate trauma services, orthopedics, and pediatrics alongside maternity at the Saudi hospital—many other journalists only focused on MSF press releases. They told the international community, falsely, that there were no more hospitals left.
The MSF team issued another press release about the 10 June attack on South Hospital. Their coverage, thanks to their local team, had been strong, yet in the rush, they announced that when South Hospital was forced to close due to the attack, there were no other hospitals left with the highest quality equipment and operating theaters. Their clarity was truncated.
Everyone in El Fasher, and most internationals following the situation closely, knew that the Saudi hospital and its Butterflies were now absorbing South Hospital’s evacuated intensive care and surgical patients.
However, major outlets like the BBC , The New Humanitarian, and others misunderstood the MSF release, claiming there were no more hospitals left.
According to our interviews and research, there are indications this may have led UN and INGO decision-makers in Geneva and New York to then triage El Fasher healthcare, assuming the city was lost
“South Hospital was one of only two with surgical capacity,” MSF told us with nuance that larger newsrooms seemed to have misinterpreted. “It was the main referral hospital for treating war-wounded in El Fasher and the only one equipped to manage mass casualties.”
Up to that point, MSF reported that “over 1,300 casualties sought treatment there.” In following press releases, they clarified that, indeed, the long ignored Saudi hospital was now the most important facility absorbing the war wounded.
While most other agencies shifted efforts toward the border or to the Tawila transit points, MSF, RI, DPDO, and ALIMA remained, and Save the Children still funneled some assistance to local partners. Local medical teams felt the dramatic reduction in effort.
Dr. Izzeldin finally called me in mid-August to offer an exclusive interview about what had happened and what their urgent needs were city-wide, as other press and aid agencies had stopped asking him for interviews since then. Not only the international aid agencies but also the media and advocates had abandoned them, he felt.

VII.
Humanitarian aid agencies and donors worldwide have often overcome war sieges to provide assistance. Since the 1967-1970 Biafra War in Nigeria; the 1992-1995 Bosnian War sieges of Sarajevo, Dobrinja, Gorazde, Srebrenica, and Zepa; the 2007-2012 encirclement of Mogadishu, Kismayo, and Baidoba in Somalia, and other cases, the UN has coordinated aid by first negotiating access for humanitarian convoys.
When blocked by fighters, flooded roads, or destroyed bridges, they arranged air drops of supplies. More recently, in places like Ethiopia and Nigeria, teams delivered medical supplies by drone carriers, even where “white hat” drones crossed air space patrolled by “black hat” drones used by armed groups. Additionally, cash transfers have often worked, allowing trapped teams to use electronic credit or cash to buy local supplies.
In Sudan, the war has been brutal, and many international governments and donors are cautious to let their support help either side, and yet the local Emergency Response Rooms (ERR)—networks of Sudanese civil society workers aiming to help communities while remaining impartial on political matters—have done wonders with mobile cash transfers.
In El Fasher, medical directors like Izzeldin and Modther have pleaded for mobile app cash transfers to buy local supplies. Even where warehouse stores were depleted or burned, local escapees would sometimes sneak back in with medicines bought at clinics and pharmacies in neighboring countries. However, donors have been highly reluctant to support this in Sudan, even as scores of people die from preventable illnesses, malnutrition-related conditions, or wounds that would otherwise not be fatal.
During separate phone calls with Izzeldin and Modther, I asked them what was still possible. Both argued that while the Geneva talks stalled over allowing humanitarian and food convoys in, and although the border has been opened, there are still flooded roads.
Despite this, there are opportunities to save lives by sending medical supplies from Port Sudan via SAF air drops and conducting mobile app cash transfers, which can be closely monitored for accountability.
In this context, Modther and I discussed over the phone how a larger agency or new donor could potentially arrange, through DPDO or Relief International, an air drop of medical supplies, if not cash transfers.
Saif at DPDO had figured out a method and had a connection. They just needed a donor with enough resources to cover the costs of such an operation, which could save countless lives. Few donors have been willing to step up, and only a few have followed through with other agencies focusing on field clinics so far.
On 24 June, right after Modther and I discussed this possibility, fighters fired rockets directly into the Saudi hospital’s pharmacy building, destroying vast quantities of medication and fatally wounding the pharmacist, another of the young women doctors who had graced the halls of Saudi.
Dr. Amna Ahmed, whom many knew through the rotations or from discussing how to trust alternative medications would be safe for patients, had worked not only at the Saudi hospital but also with Izzeldin at South Hospital.
With Sajida, Musa, and now Amna gone, and many others wounded, El Fasher’s medical teams—shrinking as most fled—became a smaller but more unified force, determined to survive.

VIII.
By July, as Eilaf, Aisha, and Mo made it to Uganda, Afrah to Chad, and Abubakr to Oman, the Saudi Hospital—now combining the emergency, surgical, pediatric, and maternity teams under one roof, with Izzeldin, Modther, and others working together, and Dr. Eman among the remaining Butterflies—was being targeted so intensely that they finally resorted to digging a new bomb shelter and trenches in the same space where women had long came to deliver babies.
Then after a brutally long drought season, the shock rains came. Beyond the new shelter taking in water, this also meant that the wounded and malnourished patients would now be joined by those suffering from malaria.
MSF at last clarified its earlier statement, and the international press corrected its reporting on the siege of El Fasher, acknowledging that the Saudi maternity team was still operating and in urgent need of assistance:
“As a result of these incidents, the Saudi hospital,” MSF announced, “which was previously a specialist maternity hospital—has become the only health facility in the city with surgical capacity and the ability to treat the wounded. Now, its ability to keep its doors open is also in jeopardy. We urgently need to bring in more supplies and more personnel to respond to this crisis, but the fighting is preventing us from being able to enter…”
In Uganda, the Butterflies look back, hoping to advocate for support for their colleagues still working in El Fasher.
“For my country, Sudan,” Dr. Eilaf says, “I think we face a very dark future because clashes are spreading to areas that were once safe. I hope they will find a way to end this violence, at least to stop these clashes for a while. Inside that terrible war, there are superheroes like my friends risking everything to save lives, but it’s not easy. We can never forget them…”
“No more conflict, running, or searches,” adds Aisha, who now stays nearby. “But to work, we have to start over and get licensed as physicians all over again. Somehow, the Sudan government must provide us with documents. Otherwise, we cannot practice medicine here. But I will try every way to start over again.”
Through the first weeks of August, Modther wrote to let me know they were being attacked again. Now and then, he and the others had been able to step out for coffee across the road or go to the mosque, but even the mosque and café had been hit recently. During one lull, staff members celebrated a wedding, complete with whatever food they could bring together, dressing up, and sharing imagery of the event online.
Nevertheless, the bombing came back again and again. Ultimately, they had to stop admitting patients, only allowing rapid in-and-out care. They had to tell people it was more dangerous to stay in the hospital than to go home.
As of 11 August, MSF reported the latest casualty numbers—likely undercounting, as many died in their homes or on the way to seek care—at 2,500 total casualties treated and 370 deaths in El Fasher’s hospitals. Many more died without reaching medical care.
Now in September 2024, with humanitarian convoys on the edge of Darfurand few donors willing to support air drops or cash transfers, RSF forces have penetrated the city deeper than ever before. With the combined war hospital team overwhelmed but continuing their work, Dr. Izzeldin leaves us with a desperate message that their story is not yet over. They keep going.
“Even if I die,” Dr. Izzeldin said. “I will not stop providing services to my community. I want to save my people as much as I can. For the organizations, if they would like to help the community, they should reflect on what has been happening and share in their suffering. They should stop those who are preventing people from accessing healthcare and medicine. International organizations should not leave these people behind. These are human beings.”

*Reem is a pseudonym for the patient who remains anonymous. Dr. Samar is a pseudonym for one of the doctors we interviewed and are still in touch with who evacuated but is still inside Sudan.
**This story has been supported by the International Center for Journalists as part of a series on health innovation.